785
Views & Citations10
Likes & Shares
INTRODUCTION
Endometrial cancer is a malignancy of the uterine lining which occurs most often in women from 50-65 years of age [1]. The estimated survival rate remains between 75 to 90 percent. Cervical cancer is the abnormal growth of cells in the cervix. These abnormalities are first apparent in the endocervix – the narrow canal that leads from inside the uterus out to the vagina [2]. The endocervical canal is the most likely vulnerable site to cancer because it is an area of cellular transition and constant change. The cervical cells are squamous cells. The endocervical canal is the point at which two cell types meet. Here the cuboidal cells actually transform into squamous cells. The intense cellular activity leaves this area susceptible to abnormalities. In the United States, the cervical cancer is the 8th most common cancer in women. In UK it is the 12th most common form of cancer in women. In European Union there were about 34000 new cases of cervical cancer reported annually [3]. In Canada 1300 women were diagnosed with cervical cancer in 2008. In Australia there were 734 cases of cervical cancer registered. In India more than 2.5 million cases have been estimated per year and it is presumed to be one of the ten leading causes of death. The cervical and breast cancers were predominant in women. The national cancer registry and a survey attributed various socio-economic and endogenous factors as the prime cause of uterine – cervical cancers in India. In contrast to the above statistics which is a decade back, the current information reveals that cervical cancer is found worldwide 5,70,000 new cases in 2018 and about 90% of deaths from cervical cancer occurred in low and middle income countries.
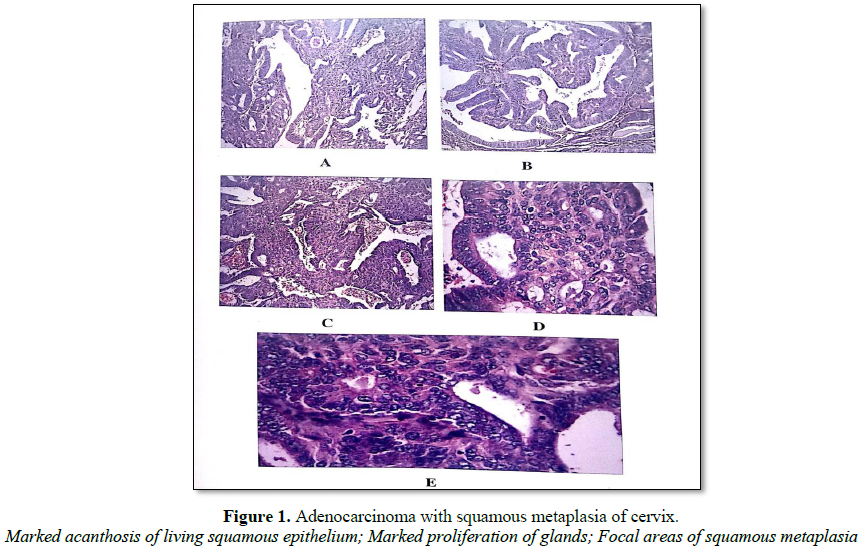
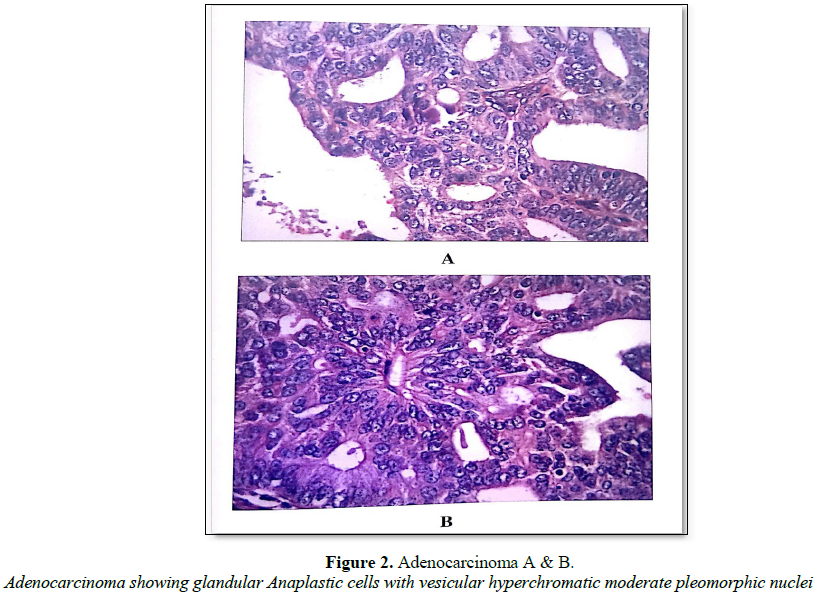
Both the preclinical and advanced stages of cervical cancers could be identified by the cyto-diagnosis. The uterine-cervical cancers have been categorized through histological examination into specific types. The various types of cervical cancers include interstitial, signet-ring cell adenocarcinoma, adenomalignum, villoglandular, pappilary adenocarcinoma, endometroid adenocarcinoma and papillary serous adenocarcioma.
ETIOLOGY
The manifestation of malignant uterine cervical cancer is a slower process of transformation and the causes are much harder to pin down due to the long latent period between the initial and final stage of manifestation. However very reasonably attributed causes are the following:
Viruses
Viral infections such as Herpes simplex virus (HSV) and Human papilloma virus (HPV) which cause premalignant change and dysplasia of cervix. Studies have revealed that Human papilloma virus can induce centrosome duplication, genomic instability and centrosome abnormalities leading to cervical cancers. In this context female partners can acquire the virus through male’s penile HPV infection, during coitus is of interest to mention [4,5].
Cholestrol
Cholesterol build up in blood and tissues is another cause for the uterine-cervical cancer. In our study, high percentage of cholesterol ranging from 47.57% to 85.02% was found in the uterine-cervical cancer tissue samples. Cholesterol derived estrogen causes endometrial hyperplasia and endometrial in situ carcinoma. Recent research in Simon Frasher University has revealed that cholesterol binding puts the brakes on oxosterol related proteins ability to couple phosphatidyl inositol-4-phasphate and accelerates cellular metaplasia and anaplasia [6].
Excess estrogen
Excess intake of estrogen over a long period of time can overstimulate the uterus lining (endometerium) and may cause an excessive thickening called endometrial hyperplasia which leads to cancer in susceptible women when left untreated. Estrogen prescription without progestrogen in HRT proved dangerous [7]. Besides the above well-established etiological reasons, life style and socio-economic status of individuals and self-hygiene could be cited as enhancement factors.
PREVENTION
· In primary prevention the uterine-cervical cancer could be prevented by knowing the above mentioned causative factors and thereby eliminating them.
· By building the active immunity through vaccination as well as by nutrition and exercises.
· HPV are found to cause genital warts which implicate premalignant and dysplasia of the cervix. Going for treatment is suggested.
· PAP test will cause a dramatic fall in death rates in promiscuous women for cervical cancer. PAP smear test is a means of secondary prevention for cervical cancer.
1. Proctor RN (1995) Cancer Wars. New York: Basic Books, p: 368.
2. Rajeswari T (2011) Studies on epidemiology, histopathology and genetic details of uterine cervical cancer in south Indian women with supplementary cell line observations and statistical modeling. Ph.D. Thesis, University of Madras.
3. Arbyn M, Autier P, Ferlay J (2004) Burden of cervical cancer in the 27 member states of the European Union: Estimates for 2004. Oxford J Med Ann Oncol 18: 1423-1425.
4. Castellsague X, Bosch FX, Muñoz N, Meijer CJ, Shah KV, et al. (2002) Male circumcision, penile humen papillomavirus infection, and cervical cancer in female partner. N Engl J Med 346: 1105-1112.
5. Duensing S, Munger K (2003) Centrsome abnormalities and genomic instability induced by human papillomavirus oncoproteins. Prog Cell Cycle Res 5: 383-391.
6. Ramalingam K, Anbarasu A, Paulraj K, Karnan P, Kanagavalli S (2019) Lipidomic therapy to cancer: A novel drug designing strategy – A research note. J Cancer Sci Treatment 1: 42-46.
7. Lila E Nachtigall LE, M.D, Heilman JR (2000) Estrogen. Harper Collins Publishers. 3rd Edn.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Spine Diseases
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Clinical Trials and Research (ISSN:2637-7373)